
In-depth research into the origin of type 1 diabetes
Thanks to generous donations to the Hippo & Friends type 1 diabetes fund and the non-profit organization Hippo and Friends, the diabetes team, led by Prof. Dr. Chantal Mathieu, Prof. Dr. Kristina Casteels, and Prof. Dr. Pieter Gillard, can conduct more in-depth research into the origin of type 1 diabetes, which in time can lead to more targeted treatment for patients and hopefully also to the prevention of the disease. At KULeuven, we work together with various international groups and industry to achieve useful results faster. In addition, the diabetes center works closely with UZLeuven so that basic research can be translated into clinical studies more quickly. A great focus is placed on translational research that makes the link between 'bench' and 'bedside'. There are various lines of research, including RNA and protein research in human cells, which aims to find new biomarkers to detect and monitor type 1 diabetes faster and better, but also to prevent and treat this chronic disease. These are ambitious goals, but we are aiming for nothing less than a world without type 1 diabetes. In addition, the KULeuven team coordinates INNODIA, one of the largest European consortia working on type 1 diabetes. In this way, there is immediate availability of human samples from patients and their relatives for translational research.

Research into immunological biomarkers
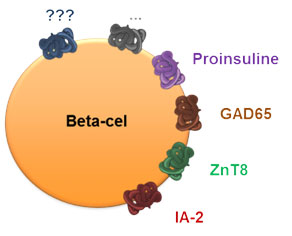
Research into immunological biomarkers for the early detection but also for a more targeted treatment of type 1 diabetes is reaching cruising speed. Some of these biomarkers, such as autoantibodies, are well established but not sufficiently sensitive to reveal the heterogeneous disease process in different individuals.
The protein research in human insulin-producing beta cells focuses on finding proteins that change in the insulin-producing beta cells in response to inflammatory reactions (inflammation) or other types of stress and thereby themselves contribute to triggering erroneous immune responses against the beta cells. cell. Some of these altered proteins move to the cell surface, making the beta cells more visible to the immune system (link). These findings were first established in mice with type 1 diabetes (link) and later in type 1 diabetic patients (link). Recently, we have also started to introduce very new technologies in the diabetes center. Single-cell RNA sequencing makes it possible to look at the entire transcriptome per cell.
Neutrophils
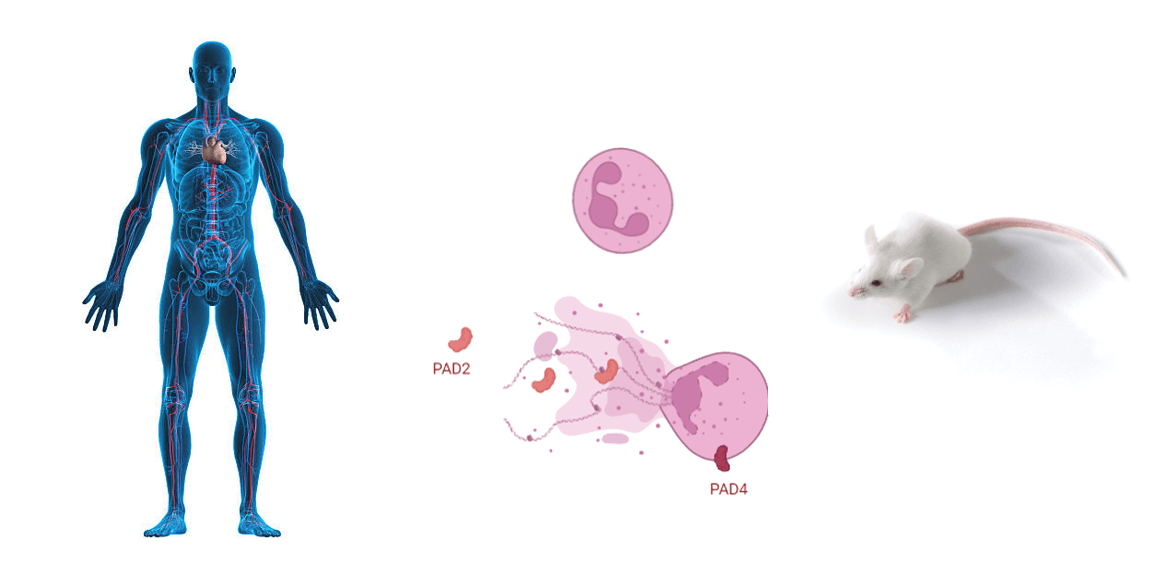
Currently, it is proposed that type 1 diabetes is mainly caused by the adaptive immune system and more specifically by the beta-cell-specific auto-reactive T cells. These invade the islets of Langerhans in the pancreas where they trigger an inflammatory response that results in influx of other immune cells and the production of chemokines, cytokines and other molecules. Recently, interest in the role of neutrophil granulocytes in the disease process of type 1 diabetes has arisen based on studies with patient samples and mouse models of type 1 diabetes. However, it is unclear how neutrophil granulocytes contribute to the onset and progression of the disease. There are also data from other autoimmune diseases showing that neutrophil extracellular traps (NETs) play an important role in the disease course of these diseases. A NET is a kind of sticky web of DNA strands. A neutrophil can shed this web to trap bacteria. Unfortunately, not only bacteria can stimulate neutrophils to make NETs, but also substances in the blood of people with autoimmune diseases can activate NETs. In the diabetes center at the KULeuven, neutrophil granulocytes from humans and mice with type 1 diabetes are phenotypically and functionally characterized using the latest technologies. How do these cells communicate or interact with the adaptive immune system and how can new insights contribute to the development of preventive and curative treatment methods?
Immune therapy
Through the gut, our immune system is exposed to a wide variety of proteins from ingested food or bacteria (intestinal or microflora). Ingested proteins do not trigger an immune attack and this phenomenon is called "oral tolerance". In collaboration with Precigen ActoBio, the diabetes center at KULeuven is investigating how proteins that are inherent to the insulin-producing beta cells can be presented to the immune system of the intestine via a genetically modified bacterium (Lactococcus lactis). It is expected that the body will tolerate these proteins and hopefully also the entire beta cell. With this approach, the disease process in laboratory animals with type 1 diabetes can be permanently stopped in 2 out of 3 cases (link; link). Based on these results, a first clinical study was started in newly diagnosed type 1 diabetes patients at the end of October 2018 (link; link).
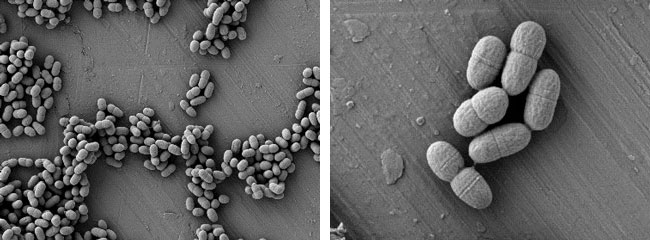
Electronmicroscopic (EM) pictures of Lactococcus lactis bacteria ©Precigen ActoBio, Zwijnaarde (Ghent), Belgium
Vitamin D

Vitamin D is a classic vitamin and hormone. Sunlight is our main source of vitamin D. Our body can make it in the skin under the influence of sunlight. A small portion comes from our diet. In addition to the beneficial effects on bone and muscle strength, we know that vitamin D is also important for the proper function of pancreas and immune system. Vitamin D protects the insulin-producing beta cells against inflammatory reactions and has a beneficial effect on the immune system, including the generation of "regulatory" immune cells that restore the balance in the disturbed immune system in type 1 diabetes (link; link). Our research has inspired scientists at the Leiden University Medical Center (LUMC) in the Netherlands and City of Hope in Los Angeles (US) and a first clinical cellular therapy with vitamin D is currently underway in diabetic patients (link; link). The KULeuven team also showed that oral vitamin D partially prevents the development of type 1 diabetes (link). The research on vitamin D focuses mainly on understanding how this vitamin can change and re-educate the immune system. Understanding this, we can potentially bring about the same changes with much more targeted drugs. Enough reason to go for a walk in the sun at least once a day for 15 minutes, but don't overdo it of course!
